LINEO TUTORIAL
NOTES OF ORTHODONTICS
THE BIOMECHANICAL MOVEMENTS
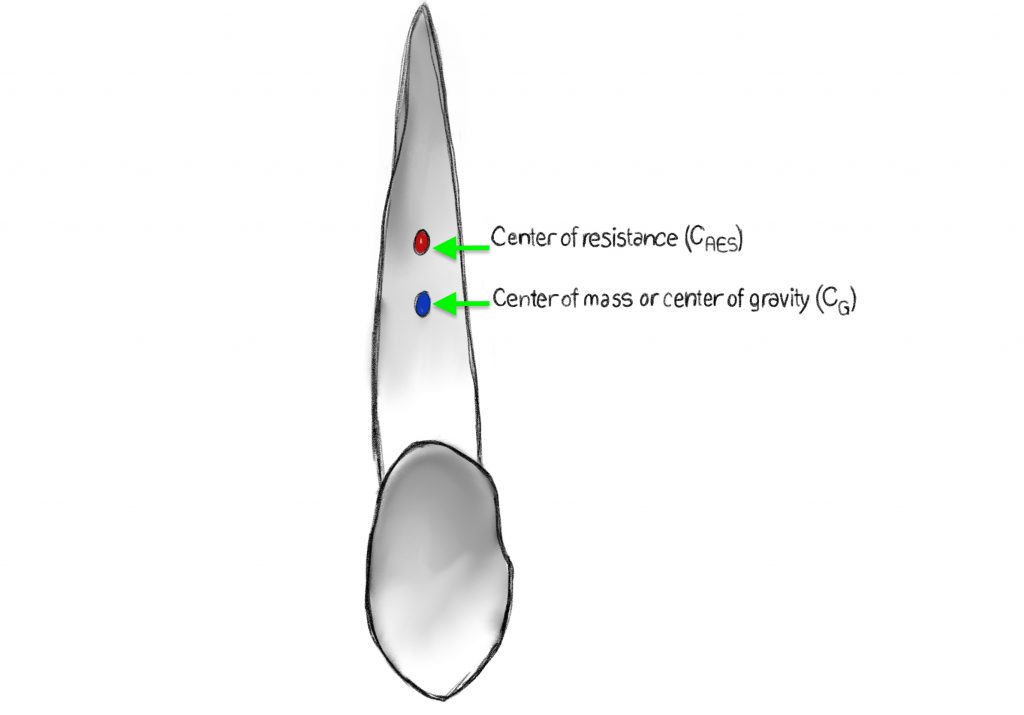
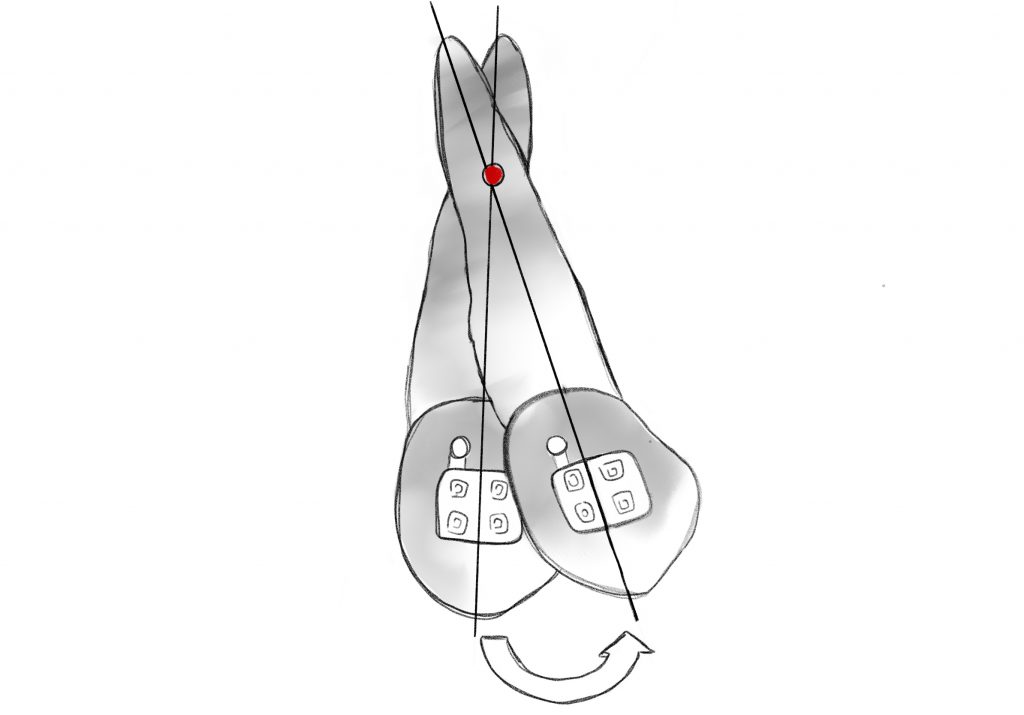
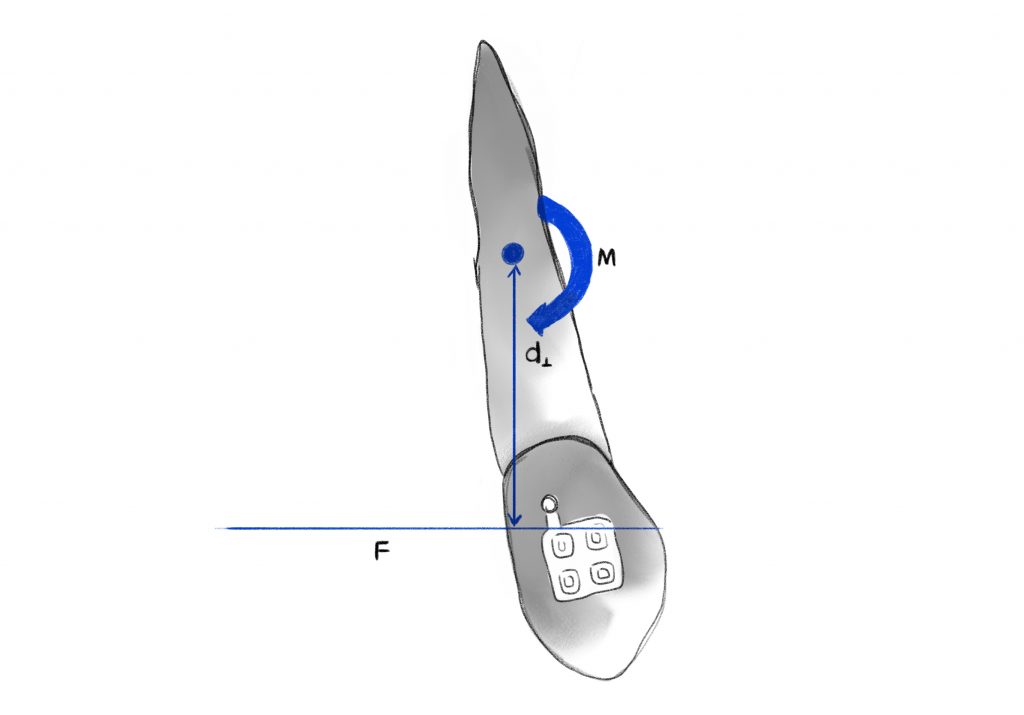
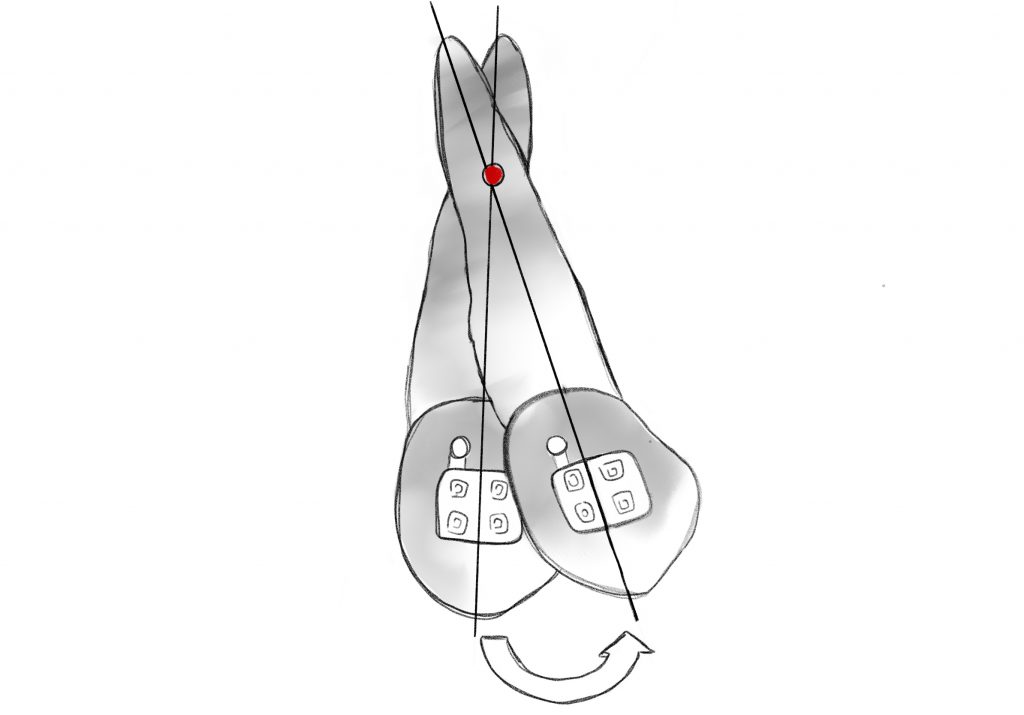
In orthodontics, biomechanics represents the application of mechanics to the biology of tooth displacement and is based on certain principles
TOOTH MOVEMENTS
FORCE SYSTEMS
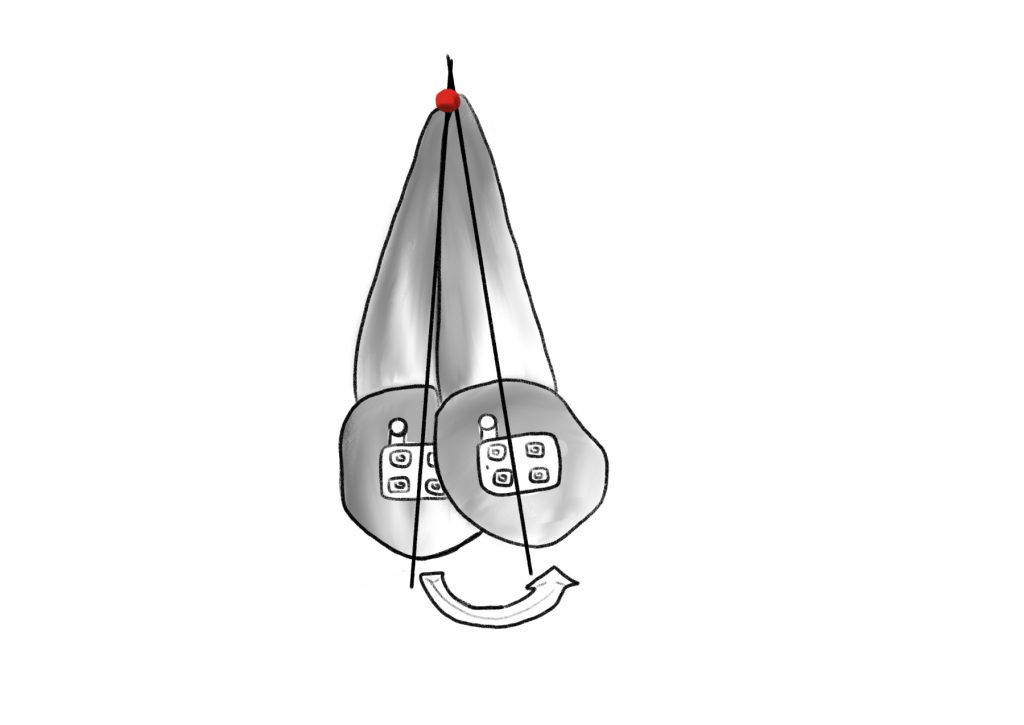
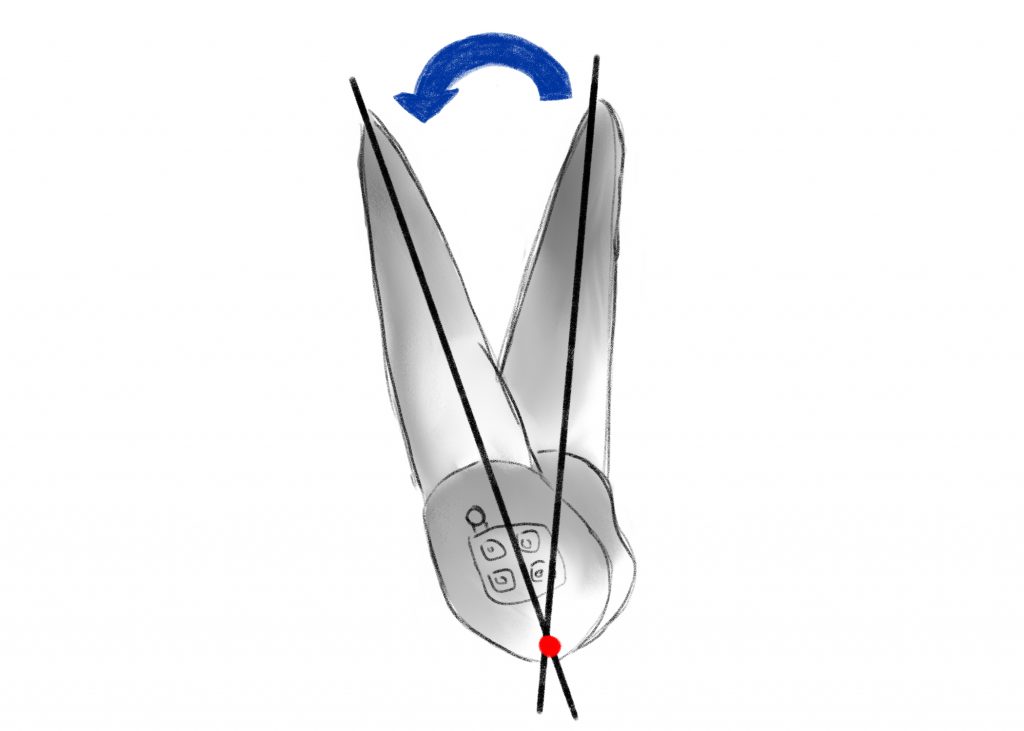
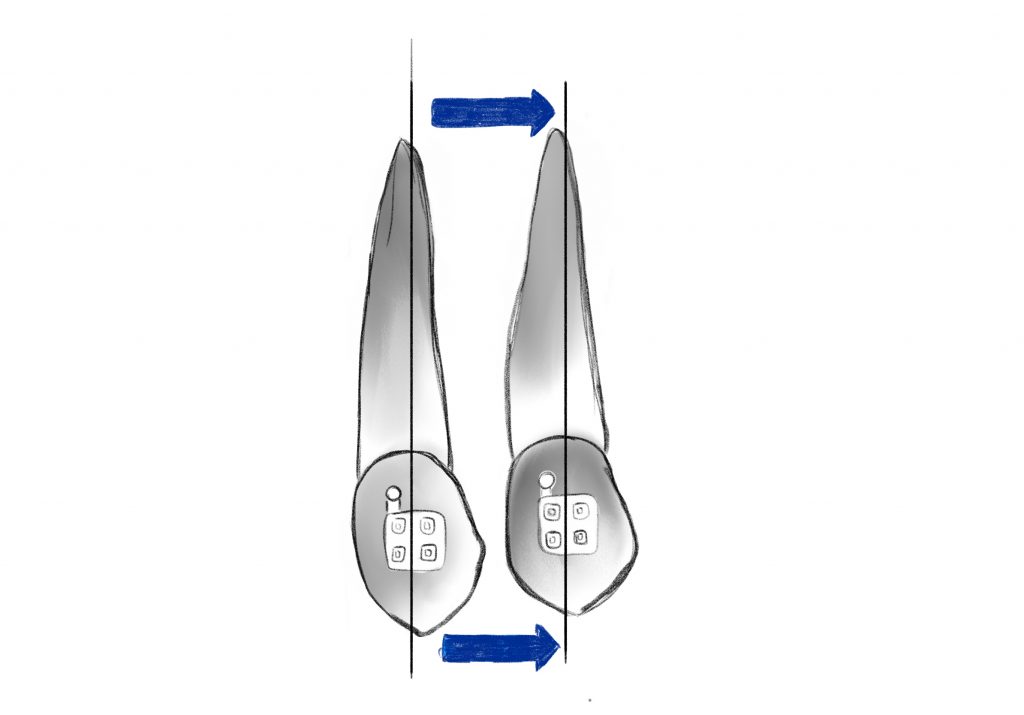
Clinically, forces can be applied in three ways to determine tooth displacement:
1.Single force that results in significant crown inclination;
2.Pair of forces that allows a controlled inclination of the root in the mesio-distal sense (tipping) or in the vestibulo-lingual sense (torque);
3.Single force + force pair, a combination that allows to obtain a translation of the tooth while maintaining good control of the root inclination.
Bibliografia
2. Davidian EJ. Use of a computer model to study the force distribution on the root of the maxillary central incisor. Am J Orthod. 1971;59:581–588.
3. Hay GE. The equilibrium of a thin compressible membrane. Can J Res. 1939;17:106–121.
4. Yettram AL, Wright KWJ, Houston WJB. Center of rotation of a maxillary central incisor under orthodontic loading. Br J Orthod. 1977;4:23–27.
5. Christiansen RL, Burstone CJ. Centers of rotation within the periodontal space. Am J Orthod. 1969;55:351–369.
6. Smith RJ, Burstone CJ. Mechanics of tooth movement. Am J Orthod.1984;85(4):294–307.
7. Pryputniewicz RJ, Burstone CJ. The effect of time and force magnitude on orthodontic tooth movement. J Dent Res. 1979;58(8):1754–1764.
8. Mulligan TF. Common sense mechanics in everyday orthodontics. Phoenix, AZ: CSM Publishing; 1998:1–17.
9. Isaacson RJ, Lindauer SJ, Rubenstein LK. Activating a 2 × 4 appliance. Angle Orthod. 1993;63:17–24.
10. Demange C. Equilibrium situations in bend force systems. Am J Orthod Dentofacial Orthop. 1990;98:333–339.
11. Koenig HA, Burstone CJ. Force systems from an ideal arch. Am J Orthod. 1974;65:270–289.
12. Burstone CJ, Koenig HA. Force systems from an ideal arch: large deflection considerations. Angle Orthod. 1989;59(1):11–16.
13. Koenig HA, Burstone CJ. Creative wire bending: the force system from step and V bend. Am J Orthod Dentofacial Orthop. 1988;93(1):59–67.
MALOCCLUSIONS
The concept of “ideal”: The purpose of orthodontic treatment is to transform a malocclusion into an “ideal” dento-skeletal Class I occlusion. The word dento-skeletal indicates that an “ideal” occlusion consists of two components (dental and skeletal).
When the teeth are in occlusion, the mesio-vestibular cusp of the upper first molar occludes in the vestibular sulcus of the lower first molar (Angle’s Class I molar ratio), with the upper canines located between the canines and the lower first premolars (Class I canine ratio).


SAGITTAL PLANE MALOCCLUSIONS




Bibliografia
1. Petroviç D, Vukiç-Culafi B, Iviç S, Djuriç M, Milekiç B. Study of the risk factors associated with the development of malocclusion. Vojnosanit Pregl 2013;70(9):817-23.
2. Bolton W.A. The clinical application of a tooth size analysis. Am J Orthod. 1962;48:504-529.
3. Moorrees CFA, Chada JM. Available space for incisors during dental development: a growth study based on physiologic age. Angle Orthod 1965;35:12-22.
4. Moorres CFA, Gron AM, Lebret LM, Yen PHJ, Frolich FJ. Growth studies of dentition. A review. Am J Orthod 1969;55:600-16.
5. Enlow DH. Handbook of Facial Growth. (2nd ed) WB Saunders, Philadelphia 1985.
MALOCCLUSIONS ON THE TRANSVERSE PLANE
A fundamental prerequisite for achieving normal occlusal relationships during orthodontic treatment is the correct positioning in the three planes of space of the maxillary bone and mandible, which must also be correctly proportioned to each other.
Under normal conditions, the right and left halves of the face are almost symmetrical and the upper arch overlaps the lower arch for its entire length. When this condition does not occur, there is a “transverse discrepancy,” which represents a “developmental abnormality in the transverse plane.” Although the diagnosis of transverse discrepancy is often straightforward, some asymmetries can sometimes be masked by dental compensations. Depending on the structures involved, these problems may have a dental, skeletal, or functional origin, or a combination of these factors may be present.
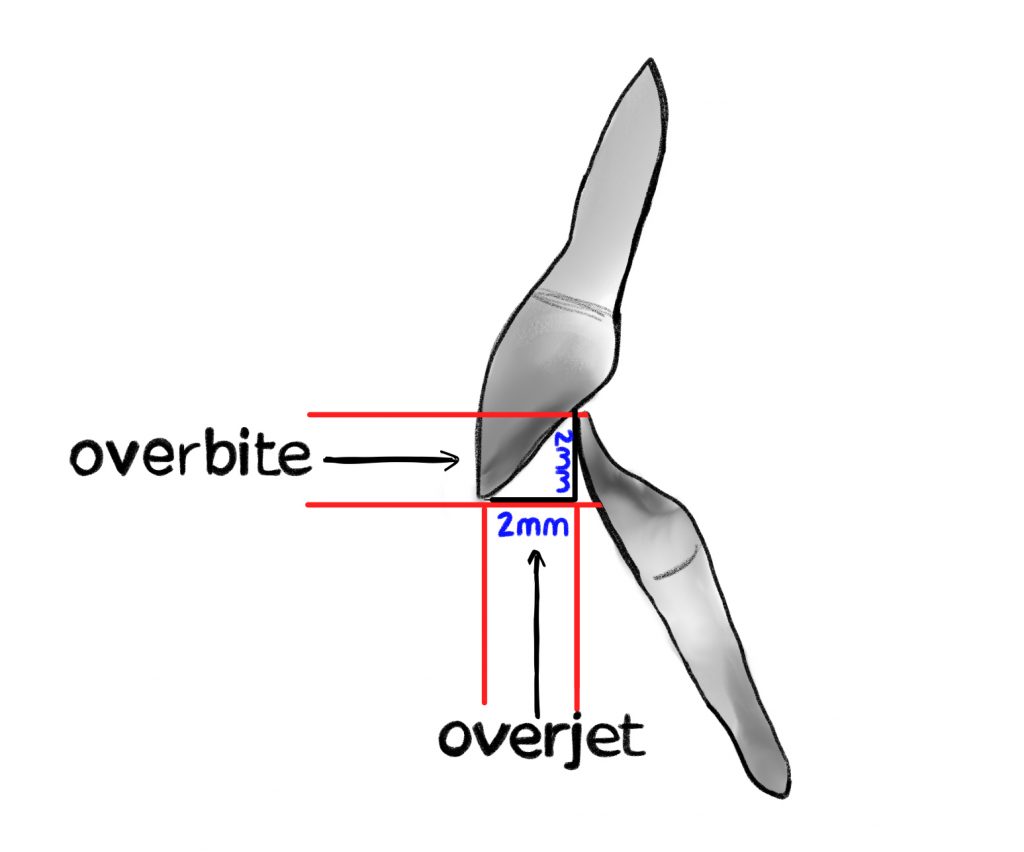
In a normal occlusion, in the transverse plane, the palatine cusps of the upper molars and premolars occlude into the pits of the lower molars and premolars while in the anteroposterior plane, the upper incisors occlude on the buccal surfaces of the lower incisors.
A crossbite represents a discrepancy in the vestibulo-lingual relationship of the upper and lower teeth. It can affect entire segments of the dental arch or individual teeth, or be mono- or bilateral. An anterior crossbite is present when the lower incisors occlude further forward than the upper incisors, resulting in a tooth relationship of complete inversion and decreased (or negative) overjet.



Bibliografia
1. Sollenius O, Petrén S, Bondemark L. An RCT on clinical effectiveness and cost analysis of correction of unilateral posterior crossbite with functional shift in specialist and general dentistry. Eur J Orthod. 2020 Jan 27;42(1):44-51.
2. Asiry MA, AlShahrani I. Prevalence of malocclusion among school children of Southern Saudi Arabia. J Orthod Sci. 2019;8:2.
3. Yu X, Zhang H, Sun L, Pan J, Liu Y, Chen L. Prevalence of malocclusion and occlusal traits in the early mixed dentition in Shanghai, China. PeerJ. 2019;7:e6630
4. Kutin, G. and R. R. Hawes. Posterior cross-bites in the deciduous and mixed dentitions. Am J Orthod 1969. 56:491–504.
5. Melsen, B., K. Stensgaard, and J. Pedersen. Sucking habits and their influence on swallowing pattern and prevalence of malocclusion. Europ J Orthod 1979. 1:271–280.
6. Linder-Aronson, S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. Acta Otolaryngol 1970. 265:1–132.
MALOCCLUSIONS ON THE VERTICAL PLANE


Bibliografia
1. Subtelny JD, Sakuda M. Open-bite: diagnosis and treatment. Am J Orthod 1964;50:337-358.
2. Mucedero M, De Toffol L, Ballanti F, Donatelli M, Cozza P. Classificazione ezio-fisio-patologica del morso aperto. Mondo Ortod 2003;1:5-15.
3. Maciel CT, Leite IC. Etiological aspects of anterior open bite and its implications to the oral functions. Pro Fono 2005;17(3):293-302.
4. Cozza P, Mucedero M, Baccetti T, Franchi L. Early orthodontic treatment of skeletal open-bite malocclusion: a systematic review. Angle Orthod 2005 Sep;75(5):707-13.
5. Jonsson T, Arnlaugsson S, Karlsson KO, Ragnarsson B, Arnarson EO, Magnusson TE. Orthodontic treatment experience and prevalence of malocclusion traits in an Icelandic adult population. Am J Orthod Dentofacial Orthop. 2007;131:8.e11–8.
6. Borzabadi-Farahani A, Eslamipour F. Malocclusion and occlusal traits in an urban Iranian population. An epidemiological study of 11- to 14-year-old children. Eur J Orthod. 2009;31:477–84.
7. Jackson S, Sandeler PJ. Fixed biteplanes for treatment of deep bite. J Clin Orthod. 1996; 30: 283-287.
8. Philippe J. Treatment of deep bite with bonded bite planes. J Clin Orthod. 1996; 30: 396-400.